The political rot eroding our national health security
The political rot eroding our national health security
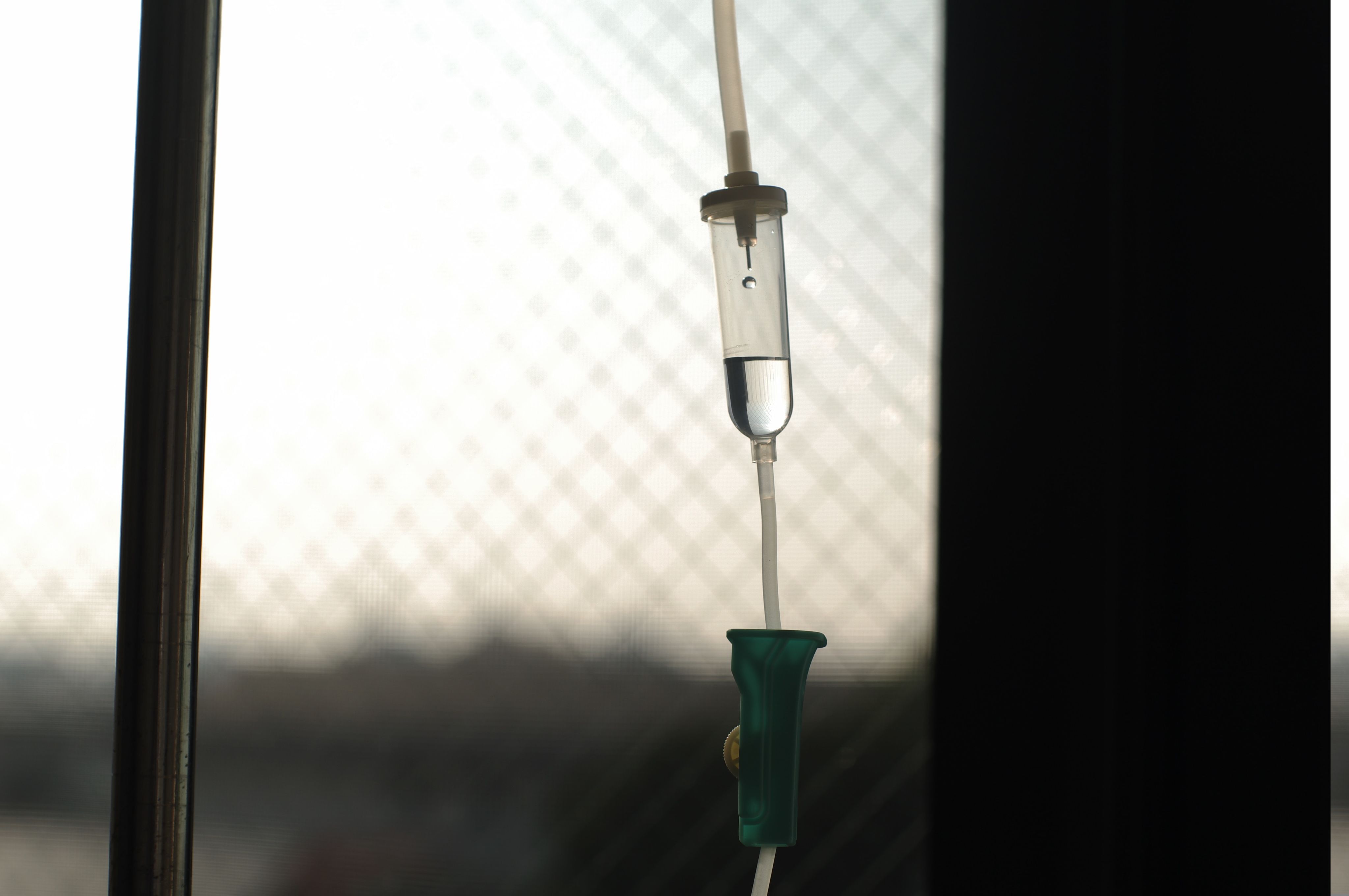
Photo by Hiroshi Tsubono on Unsplash
Photo by Hiroshi Tsubono on Unsplash
October 14, 2024
At Mass General Hospital we’re “pre-rationing” IV fluids. Hurricane Helene knocked out a North Carolina plant that provides these low-tech, high-impact supplies. Simultaneously, a never-ending carousel of medication shortages hampers our ability to care for patients, who sometimes need to forgo necessary medicines, even inexpensive generics, when they can’t afford their out-of-pocket costs at the pharmacy counter.
While seemingly unrelated, these issues have a common root cause: A political system more concerned with scoring cheap populist points than addressing real sources of our national health security crises. Policies favored by both parties’ leadership – who find it politically easier to battle made-up bogeymen than tackle real issues – threaten to undermine our national health security and eviscerate America’s world-leading innovative drug development industry.
IV fluids form the mainstay of much of what we do in the nation’s Emergency Departments and ambulances. We use them to revive home-bound elderly who are dangerously dehydrated and cancer patients with sepsis from life-threatening infections. We use them to save infants, children, and pregnant women on the edge of cardiovascular collapse from gastrointestinal illness. And we use them to stabilize trauma victims until they can be transported to hospitals for life saving transfusions or surgeries.
Shortages like this are increasingly common. In 2017, Hurricane Maria washed away a critical node in the IV fluid supply chain in Puerto Rico. In the intervening years we’ve also faced shortages of masks and other personal protective equipment, we’ve been forced to ration ventilators, and we’ve endured an endless cycle of rotating shortages of critical medicines.
The combination of escalating weather-related disasters and our aging and fractured domestic manufacturing infrastructure means these shortages will become more commonplace.
In another slow-rolling crisis, high out-of-pocket costs mean patients consistently skip critical medications. Patients who have already paid for health insurance coverage are forced by Pharmacy Benefit Managers to pay hundreds or even thousands of dollars a month for their medications – often paying many times more than the PBM did to acquire the drug.
Physicians, nurses, pharmacists, paramedics, and other healthcare workers are devising ever-more-creative ways to duct tape together a system that is falling apart despite their daily unsung heroism. But their dedication and ingenuity in the face of this absurdity risks masking how fundamentally broken our system is.
These are embarrassing and avoidable self-inflicted wounds on a national scale.
In the case of our decaying supply chain, it is politically rewarding for politicians to shout “China!” as the source of our national health security woes – as they have with the inaptly-named “Biosecure Act” which is forcing drug companies to move their supply chains from China. Ideally we wouldn’t rely so heavily on China (or any other country) for our medical supply chain.
But decades of short-sighted industrial policy and underinvestment in advanced domestic manufacturing means that an alternate on-shore medical supply chain is Washington fiction. Immigration policies that fail to attract and keep the most innovative scientists and engineers compound the problem.
Similarly, it’s easier for both parties’ populists to convince voters that “evil drug companies” are responsible for the high prices patients pay out of pocket at the pharmacy counter. This is simply false and ignores the real issues driving the problem.
Why do patients actually have to routinely choose between their prescriptions and feeding their families? Because of the anti-patient/anti-employee policies and practices of PBMs and insurers, who ultimately answer to employers (and their HR departments), who resort to opaque tricks to profit off of the very employees they are supposed to protect.
Insurers have convinced the American public that having “skin in the game” stops us from unnecessarily using up medical resources. But in my 22 years as a doctor, I have never met a patient who fakes cancer to get chemotherapy or fakes diabetes to get insulin.
Addressing our national health security disasters of fragile drug and medical supply chains and high out-of-pocket costs will require political leaders from both sides of the aisle to target our real problems: a broke and broken national manufacturing infrastructure and an HR/Insurance/PBM system that bilks the very people it’s supposed to be serving.
Policy fixes exist to spur a robust, resilient national supply chain for critical drugs and medical supplies while bolstering our pipeline of next-generation manufacturing technologies and creating thousands of high-paying, skilled jobs for the future. Likewise, there are simple steps that could address out-of-pocket drug costs while preserving our biomedical innovation excellence.
We need honest conversation and true political leadership to stand up to populist extremes of both parties. In the meantime, my frontline colleagues will continue making impossible compromises to shore up the system as long as they can. But a breaking point is coming – and they cannot continue to carry this burden alone.
About the Author:

Joshua Resnick, MD, is an Attending Physician in the Department of Emergency Medicine at Massachusetts General Hospital and a Senior Managing Director at RA Capital Management.

